“Antibodies provide the quickest pathway to beat the virus”
mAbCo19
- our insight of the week
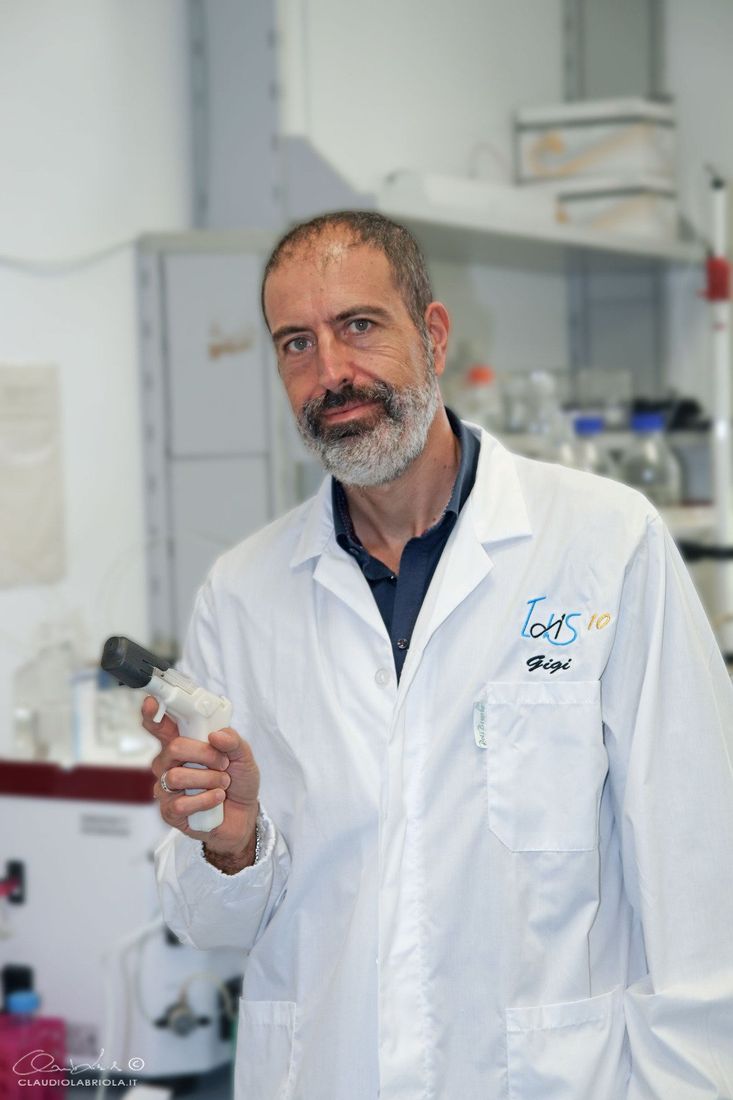
Dr. Rino Rappuoli, private photo
While scientists all over the world are looking for treatments and vaccines against Covid-19, one natural process has already managed to defeat the virus: human antibodies. Over one million patients worldwide have now recovered from Covid-19. Their immune system fought the virus off with their antibodies eventually neutralizing the pathogen. Italian scientist Rino Rappuoli wants to turn that natural immune response into an effective treatment method.
Rappuoli’s goal is to isolate the cells that produce the strongest antibodies from the blood of recovered patients and eventually manufacture them on a large scale. This way, the antibodies could be used both as a treatment for people fighting Covid-19 and to prevent infection in the first place. “It is the fastest and safest chance we have right now to fight the virus”, says Rappuoli on the phone from his home in Siena, Italy. “Because we know the antibodies work – we know that from the people who recovered.”
The immune system memorizes the antibodies that it produces in so-called memory B cells. Rappuoli and his team have isolated the cells that successfully produce the antibodies which fought off the virus. This was done by analyzing blood samples that were donated by seven recovered patients from the Lazzaro Spallanzani National Institute for Infectious Diseases in Rome.
The paper “Identification of Neutralizing Human Monoclonal Antibodies from Italian Covid-19 Convalescent Patients” released
in bioRxiv on May 8, 2020 by Rappuoli and his team shows that analyzing and isolating those cells that produce potent antibodies is in fact possible and in a short amount of time.
In less than two months, Rappuoli and his team have isolated more than 1,100 memory B cells out of the donations. 74 of these cells were able to produce antibodies that recognized the virus and slowed down its growth. More critically, 17 of these identified cells eliminated the virus growth completely. These are the ones the team was specifically looking for. Because they are so rare, a very specific and sophisticated technology was used to be able to identify these cells in the shortest amount of time possible.
This fast discovery was not coincidental. A year ago Rappuoli and a team of first two, now ten scientists started working on monoclonal antibodies in their lab in Siena, the Monoclonal Antibody Discovery (MAD) Lab. This research which focused on treatment against antibiotic-resistant bacteria was supported by the Fondazione Toscana Life Sciences together with a grant from the European Research Council (ERC). Then the novel coronavirus started to spread across the globe. With the technology and methods they had just developed, Rappuoli was immediately able to shift their research focus to analyze the antibodies from Covid-19 patients. "That’s why we were able to do everything in such a short amount of time", Rappuoli says. “Two months ago, that seemed impossible.”
Rappuoli who, apart from his work in the MAD Lab, is also the chief scientist of GSK Vaccines, is renowned for his work in the field of vaccinology. Now, at 67, he is used to dealing with emerging viruses: SARS, ZIKA or MERS. They all have one thing in common, Rappuoli says: “the world is never prepared.” But while he is certainly familiar with serious epidemics, the sheer scale and urgency of this global pandemic has put extraordinary strain on his team. “The pressure is enormous”, says Rappuoli. Right now, the days in the lab are very long, with 15 to 20 hours daily becoming the norm. “But doing a job that I know can be useful and save lives is extremely motivating. It is pushing me to work hard.”
And time is crucial in fighting the virus. Monoclonal antibodies could provide short-term protection, while a vaccine will help eliminate the novel coronavirus in the long term. Antibodies can be manufactured a lot faster than vaccines, says Rappuoli. There are already more than 50 antibody products licensed to treat other diseases like cancer or autoimmune disorders. Additionally, the manufacturing infrastructure to handle the production of such a treatment is already in place, says Rappuoli, with manufacturing capacity in Japan, China, the US, Switzerland, the UK and other places in Europe.
While monoclonal antibodies are not a replacement for vaccines which provide long-term protection, they could prevent an infection for around five or six months. And the protection through antibodies would be immediate, just one hour after injection, as opposed to vaccination where it often takes a month for the immune system to react, says Rappuoli. This is an important factor, especially for health care workers on the front line or vulnerable groups.
“Right now, we have several cells in the lab that could be the perfect candidate”, says Rappuoli. While the analysis of new blood samples remains ongoing in search of even more potent antibodies, the next steps towards the first phase of a clinical trial are already in motion. This treatment would usually take 18 months to be approved, but now with time pressing, they are aiming to reduce this process to just six. “There are no quick solutions”, Rappuoli says. “But from experience we know which risks to take and what corners we cannot cut.”
May 8, 2020 by kENUP Foundation
Biography Rino Rappuoli
Press release by the European Patent Office
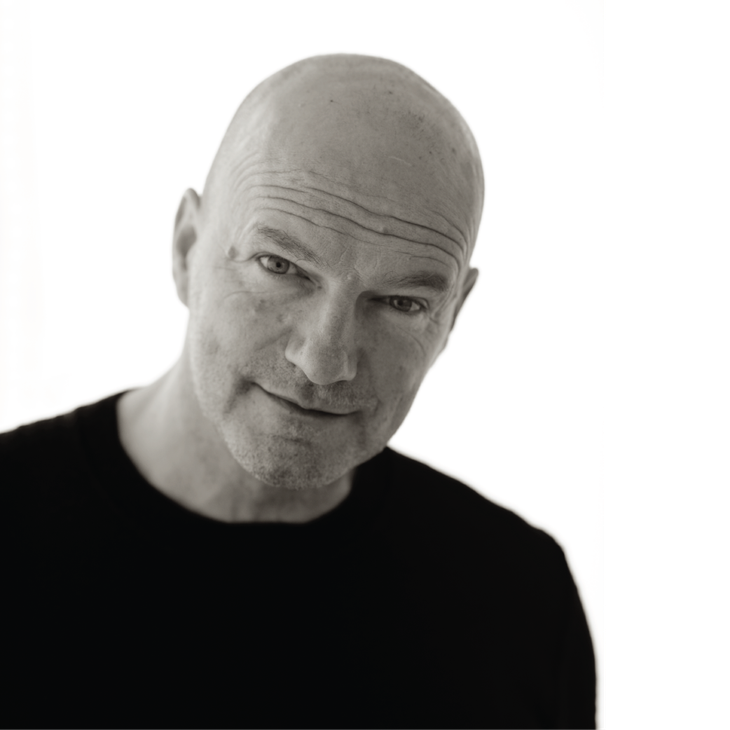
The father of modern-day vaccinations: Rino Rappuoli receives European Inventor Award 2017 for Lifetime Achievement
Venice/Munich, 15 June 2017 - Infectious diseases such as diphtheria, bacterial meningitis and whooping cough have essentially been eradicated in the developed world, thanks to a new generation of vaccines invented by Rino Rappuoli (65). Over the course of a research career spanning more than 40 years, the Italian microbiologist from the town of Siena has pioneered numerous life-saving immunisations and advanced laboratory techniques for their manufacture. His patented inventions are administered to millions worldwide in routine vaccination programmes. For this accomplishment, the European Patent Office (EPO) honoured Rappuoli with the 2017 European Inventor Award in the "Lifetime Achievement" category, one of five award categories, at a ceremony held today in Venice.
"Rino Rappuoli's innovative vaccinations and techniques have made the world a safer place," said EPO President Benoît Battistelli. "His genomics-based vaccines have saved millions of lives around the world. They have vanquished several diseases and created a new school of vaccine design."
The award ceremony at the Arsenale di Venezia was attended by some 600 guests from the areas of politics, business, intellectual property and science, and opened by the EPO President together with Carlo Calenda, Italy's Minister of Economic Development.
The award, now in its 12th year, is presented annually by the EPO to distinguish outstanding inventors from Europe and around the world who have made an exceptional contribution to social development, technological progress and economic growth. The winners were chosen by an independent international jury from a pool of more than 450 individuals and teams of inventors put forward for this year's award.
A new way to engineer immunisations
In the 1990s Rappuoli and his team completely changed the way vaccines were developed. Before his inventions, vaccine design had followed a blueprint established by French microbiologist Louis Pasteur in the 1880s: doctors inject patients with "weakened" versions of infectious organisms, allowing the immune system to prepare a defence. However, the immune system is "blind" to many infections such as the bacteria behind meningitis - a serious illness affecting the brain. Changing the paradigm, Rappuoli applied genetic engineering to create hybrids between bacterial DNA and proteins to attract the immune system's attention. It was a watershed. When the first "conjugate vaccine" against whooping cough became standard in Italy in 1993, the disease was eradicated within two years. The same happened when Rappuoli's meningitis C vaccine, for which he tapped genome pioneer Craig Venter to DNA-sequence bacteria, became part of the UK's immunisation scheme. The underlying process of "reverse vaccinology" forever changed vaccination design. "Vaccines are now no longer based on grown agents, but are designed on the computer using genomics," says Rappuoli. He made history by developing and patenting the first-ever vaccines for each strand of meningococcal meningitis - namely A, B, C, Y and W-135 - that have been approved world-wide.
Making an impact
Rappuoli's life's work has enabled him to leave a mark. "I spent most of my life working in company-owned research institutes, because there you can go beyond the paper and translate your discovery into real products that can have an impact on people," he says. Patented inventions such as his anti-meningitis B vaccine Bexsero are used worldwide, generating annual sales of approximately EUR 465 million for its license holders. Their underlying laboratory techniques, for which Rappuoli holds around 150 granted and pending European patent families, have also unlocked new fields of scientific development. Meanwhile, Rappuoli has also set up a global health institute devoted to developing vaccines for which there is no market, but for which there is a huge medical need in low-income countries. Through the institute, the patents, know-how and technology can be made available free-of-charge: "With vaccines, life expectancy can be increased and the gap between rich and poor reduced," he says.
A lifetime of fighting infectious diseases
One of the most influential careers in microbiology was inspired by the devastating effects of pandemic infections. The unfinished cathedral wall in his native Siena - a remnant of the year 1348, when the "Black Death" ravaged the city - set Rappuoli on his course: "Such a thing should never happen again, so I decided to devote my entire life to the development of vaccines." Over the years, Rappuoli's contributions have been recognised with the highest honours in the field of medicine, including the Italian Gold Medal for Public Healthcare. But his work is never finished. As the Chief Scientist at global pharmaceutical manufacturer GlaxoSmithKline (GSK) Vaccines, Rappuoli is preparing vaccines against Respiratory Syncytial virus, Cytomegalovirus and other potentially devastating infections: "I believe there is no better job in the world," the microbiologist says.