OraCOV
is an oral, self-administered vaccine candidate against COVID-19.
Under development by by Sanaria Inc., Protein Potential, LLC, and the Institute for Tropical Medicine, University of Tübingen
OraCOV
OraCOV is an oral, self-administered vaccine candidate against COVID-19. OraCOV comprises multiple SARS-CoV2-specific antigens in a formulation that is easily manufactured, safe, and effective. More than 150 million doses of the vaccine formulation platform have been safely administered worldwide in the past 3 decades.
This formulation is orally self-administered in 3-4 doses over 4-6 days, has an excellent safety record, and induces protective immunity for 3 to 7 years mediated in part by antibodies and cellular T cell immune responses.
Most human vaccine formulations require refrigeration for storage, and several visits to a clinical setting for administration. OraCOV will: 1) be stable at room temperature; 2) be self-administered at home; and 3) induce secretory IgA antibodies and protective T cell responses to interdict SARS-CoV-2 at the respiratory mucosa. We have used this formulation and vaccine approach to produce vaccines that protect against lethal inhalational anthrax in rabbits, shigellosis in mice, and enterotoxigenic Escherichia coli diarrheal disease in mice.
Development, characterization, and manufacturing are expected to be completed in mid 2021, and clinical trials in Germany will begin immediately thereafter. Leveraging their experience in vaccine development, infrastructure, manufacturing, and regulatory and clinical affairs, and their collaborators and advisors, Protein Potential, Sanaria, and their partners at the University of Tübingen are well positioned to develop, manufacture, test, license, and deploy OraCOV vaccine.
What a second generation of Covid-19 vaccines could do differently
our insight of the week - December 5, 2020
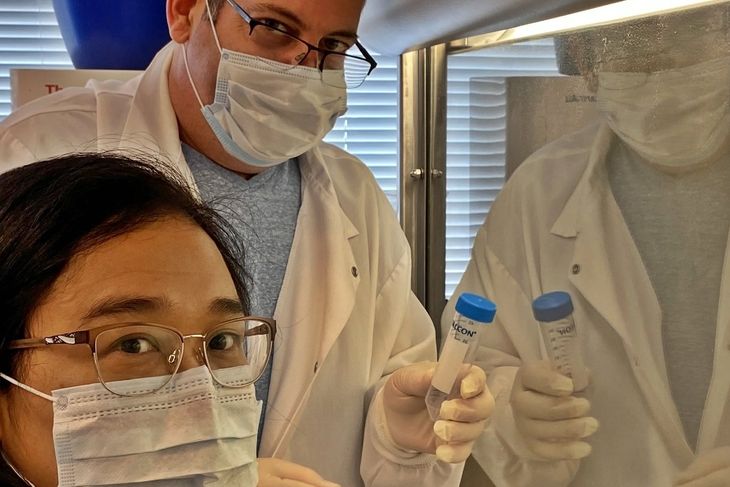
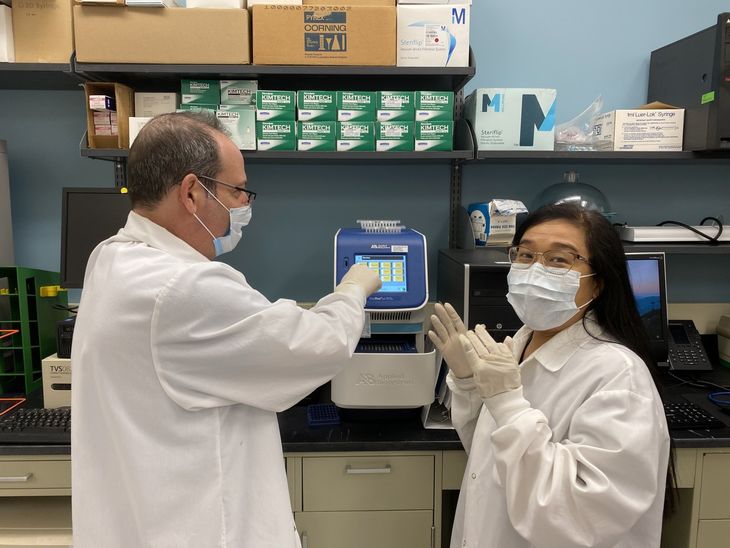
Dr. Ehud Inbar and Ms. Tint Wai working on OraCOV, photo courtesy company
In the past weeks, three Covid-19 vaccine developers have released their first promising results. Efficacies of as much as 94 percent in preliminary data turned out to be more than what was expected. Even to other vaccine developers like Stephen L. Hoffman, CEO and CSO at U.S. biotechnology company Sanaria, this was a surprise. Sanaria is currently developing a vaccine candidate called OraCOV. “Those results from other developers are very exciting because now it’s proven that the form of spike protein used is effective in inducing protective immune responses, at least in the short run”, he says on video call from his office in Rockville, MD, U.S. It is also promising news for Sanaria’s development, because OraCOV uses a similar form of the spike protein, as Hoffman explains. But there is also a question lingering now that a lot of vaccine developers have to ask: “What is the world’s appetite for a second generation of Covid-19 vaccines?”, Hoffman says.
There are still a lot of unknowns with any vaccine candidate: Will the final results turn out as good as the preliminary ones? Will it be possible to manufacture and transport millions or even billions of doses? Right now, all of the candidates with first results require a cold chain, some of up to -80 degrees Celsius. And a third unknown that a lot of people have started to worry about: Will the whole world benefit from it, or just the strongest economies?
“I don’t mean to diminish those enormously exciting results in any way”, Hoffman explains. “But we all know from long experience in vaccine development that it would be great to have an additional approach that is potentially more practical in the future.” That is why he deems it critically important to still pursue OraCOV and other candidates, even if everything works out with the current generation of vaccines.
Dr. Ehud Inbar and Ms. Tint Wai working on OraCOV, photo courtesy company
OraCOV’s approach differs from the ones currently tested in four significant ways. The first one is in the administration: instead of through injection, OraCOV will be administered orally. People would even be able to self-administer it by dissolving it into a glass, swishing it around their mouth and swallowing it. Through this approach, the vaccine comes in touch with the membranes lining the mouth and throat directly, where the SARS-COV2 virus usually enters. Therefore, the initiation of the protective immune response actually takes place where it is most needed.
The second is the time to immunize. Most of the vaccines under consideration will require two doses administered during three to four weeks. It is anticipated that immunization with OraCOV will be completed in 6 days.
Thirdly, OraCOV could be shipped in a sachet in an ordinary envelope at room temperature. This means it would not require the extreme cold chains of many other vaccines, also avoiding the expenses associated with that mode of transport, as Hoffman explains.
And fourth, Sanaria is including three of the virus’ proteins in OraCOV, not just one like other vaccines. This could lead to backing up the immune response even further which could mean more durable and broad immunity in the long run.
And, Hoffman adds, there is also the far future to think about. “We weren’t ready for this pandemic, even though the public health community has been predicting something like it for decades”, Hoffman says. “So, let us provide a foundation for the next round – which we hope will never come, but we have to be prepared.”
Hoffman expects that the decision whether or not to start clinical trials on OraCOV in the course of 2021 will be made in the next six months. At that point, not only will they have more insight on OraCOV’s performance itself, but also on the vaccine uptake and success in the rest of the world. “If we succeed in having a room temperature stable, highly effective vaccine that can be administered by drinking it as planned, that would be a tremendous practical advantage”, Hoffman says. “Particularly for the parts of the world that don’t have the funds or infrastructure to deliver the kind of vaccines that are talked about right now.”
December 5, 2020 by kENUP
OraCOV – It’s in the name – an oral vaccine for self-administration
our insight of the week - September 1, 2020
Dr. Ehud Inbar and Ms. Tint Wai working on OraCOV, photo courtesy company
A malaria vaccine developer, Sanaria is joining the fight against Covid-19
Sanaria is an ambitious biotech company that is successful because it is unique. Sanaria is developing highly effective and safe malaria vaccines designed to eliminate malaria from geographically designated areas – and now, harnessing its capabilities it wants to develop and distribute a vaccine against Covid-19 that is administered differently from most of the candidates currently under investigation, namely orally, like a drink.
This is the ingenious idea that Dr. B. Kim Lee Sim, and Dr. Stephen L. Hoffman, Sanaria's Executive VP Process Development and Manufacturing, and Chief Executive and Scientific Officer, respectively, and their team at Sanaria are hoping to make a reality through OraCOV.
The name is a portmanteau word based on oral, reflecting the idea that this vaccine would be administered through the mouth, and Covid-19, and, as Dr Hoffman explained in conversation, the Sanaria brand derives from a similar logic.
Dr. Ehud Inbar and Ms. Tint Wai working on OraCOV, photo courtesy company
Back in what seems like another (pre-coronavirus) age, in 2003, Sanaria began life with that mission to develop a malarial vaccine with a fitting company name - malaria is Italian for bad air while sanaria means healthy air.
Its most advanced antimalarial vaccine, PfSPZ Vaccine, was due to start Phase III clinical trials this year, but this timeline has been delayed because of the coronavirus pandemic. Previous indicators had shown that the malaria vaccine the company is developing would be more effective than any others in development, so Hoffman has high hopes that this standard will be replicated in OraCOV.
Sanaria, based in Rockville, Maryland, in the US and active in multiple East, West, and Central African countries in the battle against malaria is now working with its sister company Protein Potential, which makes vaccines against enteric diseases and bioterrorism agents, in collaboration with the University of Tübingen in south-west Germany on this project.
So, why an oral vaccine? Dr Hoffman says he wanted “to do something different to complement the other vaccines, take a different approach, with different ideas.” Almost all the other companies in the process of making vaccines against Covid-19 are following a similar and familiar route in that it’ll be injected into the arm and will induce protective immunity against the coronavirus through inducing immune responses first in the lymph nodes in the armpit. But, Dr Hoffman pointed out, the coronavirus is hitting people especially hard in the lungs, the throat, nose etc. so by vaccinating people through the mucosa, one should get a much faster acting and effective vaccine. The idea here will be to kill it on the surface linings of the nose, the throat, the gut and the lungs, on the surfaces where Covid-19 typically likes to habituate by inducing protective antibodies called secretory IgA and T-cell responses. The same platform, if it works for Covid-19, could also be used for other emerging infectious diseases.
And: since the oral vaccine is stored at room temperature, and it would be easily mailed, the vaccine would come in the form of a powder in an envelope, with doses mixed at home with water, and then drunk . Almost like taking a flavoured liquid antibiotic or cordial. None of the recipients would have to come to a health care facility with many other people to receive an injection.
But this isn’t the only advantage, Dr Hoffman says, because unlike other injection-based vaccines, OraCOV can be stored at room temperature, meaning that even people in the remotest parts of the world, with the most basic facilities, should have easy access to it. Other vaccines will have to be refrigerated at ultra-low temperatures and stored on dry ice, something most healthcare centres, even in Germany, are not equipped for.
Already working, like other pharma companies, at unprecedented speeds in the hope of beginning clinical trials of its vaccine in 9-12 months, its main challenge right now is to secure funding to make the progress needed. Once they secure funding, they hope to bring the vaccine from bench to bedside rapidly and save lives of people all over the world.
September 1, 2020 by kENUP